Abstract
Relationship between perioperative cardiovascular risk factors and bone marrow cells from patients undergoing coronary artery bypass grafting surgery
Author(s): L. Zhang, R. Wang, C.-S. Xiao, Y. Wu and C.-Q. GaoCell therapy through the implantation of autologous bone marrow cells has long been used in clinical trials for the treatment of ischemic heart diseases. However, as the outcomes of cell implantation vary among patients, risk factors that might influence the level and function of bone marrow progenitor cells should be determined, to identify patients who would benefit the most from this treatment. We collected clinical and laboratory data from 44 patients scheduled to undergo sternotomy for coronary artery bypass grafting (CABG). Bone marrow was aspirated from the sternum during the operation, and bone marrow mononuclear cells (BMMNCs) were isolated through density centrifugation. A negative correlation was observed between the number of BMMNCs and age (N = 44, r = -0.788, P = 0.001). The level of CD34+ cells in BMMNCs was 0.94 ± 0.39%, CD133+ cells 0.46 ± 0.28%, and CD34+CD133+ cells 0.53 ± 0.26%. The levels of CD34+ and CD133+ cells in diabetic patients were significantly lower than those in nondiabetic patients. Female gender, advanced age, and poor heart function were related with reduced progenitor cell clonogenic function. A positive correlation was observed between the level of CD34+ cells and BMMNC migration ability. Aging and diabetes were the major risk factors that influence the level and function of bone marrow resident progenitor cells in patients with coronary heart disease undergoing CABG. Further study is needed to determine whether these two factors can influence the outcome of bone marrow cell therapy for ischemic heart disease.
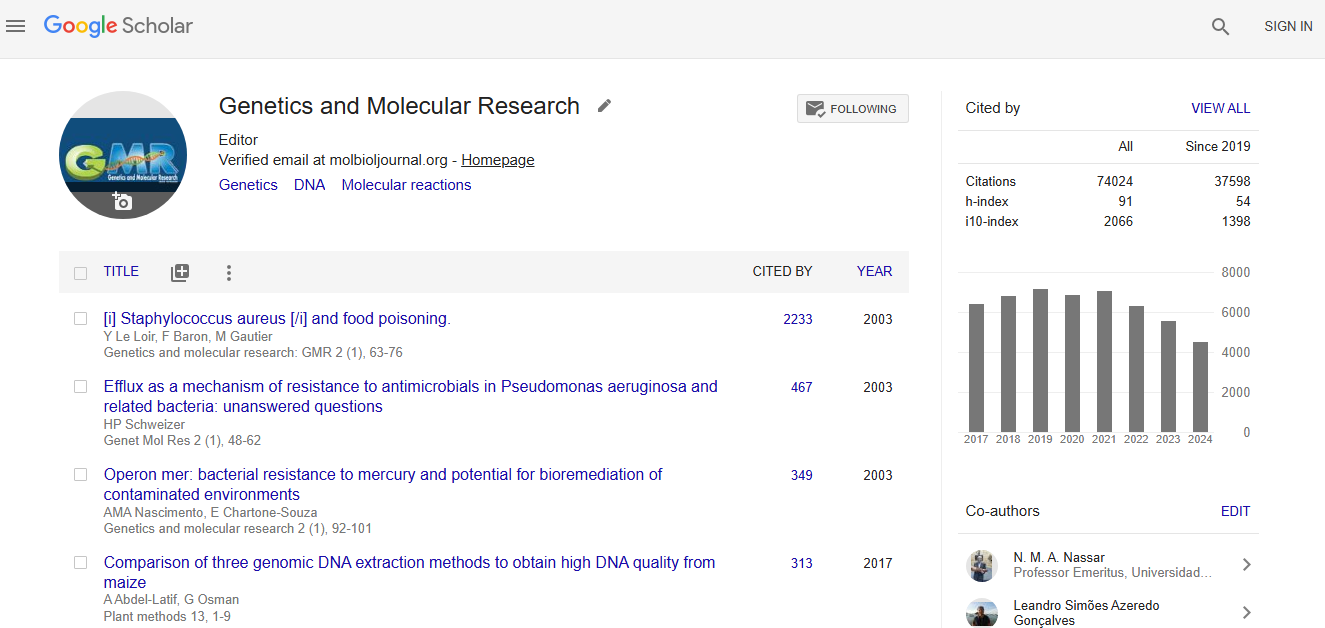
Impact Factor an Index
Google scholar citation report
Citations : 56184
Genetics and Molecular Research received 56184 citations as per google scholar report